How MMJ Health can help Patients with Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) refers to a group of chronic conditions that cause inflammation in the gastrointestinal tract. The two primary forms of IBD are Crohn’s disease and ulcerative colitis. These conditions can lead to various symptoms such as abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue.
While the exact causes of IBD are not fully understood, it is believed to involve an abnormal immune response in individuals with a genetic predisposition. When it comes to managing the symptoms of IBD, medical marijuana has shown promise as a potential therapeutic option. Fortunately, medical marijuana has shown promise in helping to manage the symptoms of IBD.

This study investigated the effectiveness of medical cannabis in managing symptoms of Inflammatory Bowel Disease and the results showed that medical cannabis use was associated with a significant reduction in symptoms such as abdominal pain, nausea, and diarrhea in patients with IBD. It also showed that most subjects had reduced their use in traditional medication. In this article, we’ll explore some of the most common symptoms and types of IBD, and what the best cannabis terpenes and strains are for you.
Furthermore, medical marijuana may provide relief from associated symptoms such as nausea, anxiety, and insomnia, which are commonly experienced by individuals with IBD. It is important to consult with a healthcare professional specialized in medical marijuana to determine the appropriate strains, dosages, and modes of administration for personalized treatment plans.

Inflammatory Bowel Disease (IBD) is a complex group of chronic conditions that affect the gastrointestinal tract, primarily including Crohn’s disease and ulcerative colitis. While the exact causes of IBD are not fully understood, a combination of genetic, environmental, and immune system factors is believed to contribute to its development. Understanding the potential causes can help individuals better comprehend the condition and explore strategies for managing its symptoms. The following are some factors that are thought to play a role in the development of IBD:
It is worth noting that while these factors are believed to contribute to the development of IBD, the precise interplay between genetics, environment and immune response is still being investigated.
Inflammatory Bowel Disease (IBD) encompasses two primary types of chronic conditions that affect the gastrointestinal tract: Crohn’s disease and ulcerative colitis. While they share similarities in terms of symptoms and the chronic nature of inflammation, there are distinct differences in the areas of the digestive tract that they affect and the patterns of inflammation. Understanding the types of IBD can help individuals and healthcare professionals tailor treatment plans and management strategies. Here are the two main types of IBD:
While they are both forms of IBD, the specific areas of the digestive tract they affect, the patterns of inflammation, and the potential complications can vary. It is important for individuals with IBD to work closely with healthcare professionals to accurately diagnose and manage their condition based on the specific type and individual needs.

The symptoms of Inflammatory Bowel Disease can vary depending on the type of IBD a person has and the severity of their condition. Recognizing these symptoms is crucial for timely diagnosis and effective management of the condition. While the specific symptoms can differ from person to person and depending on the type of IBD, there are common signs to be aware of. If you experience any of these symptoms, it is important to consult with a healthcare professional for a comprehensive evaluation and appropriate care. Here are some of the common symptoms of IBD:
To diagnose Inflammatory Bowel Disease (IBD), a doctor would typically take the following steps:

As it can be appreciated, the diagnosis of Inflammatory Bowel Disease involves a combination of clinical evaluation, laboratory tests, endoscopic procedures, imaging studies, and pathological analysis. This comprehensive approach helps healthcare professionals differentiate between Crohn’s disease and ulcerative colitis, determine the extent and severity of the disease, and develop an appropriate treatment plan tailored to the individual’s needs.
Studies have shown that terpenes, the aromatic compounds found in cannabis and other plants, may offer therapeutic benefits for individuals with Inflammatory Bowel Disease (IBD). Here are some of the best terpenes for IBD and their potential benefits:
has anti-inflammatory and pain-relieving properties and may help reduce anxiety and depression.
Known for its calming and relaxing properties, linalool may help reduce anxiety and provide pain relief. It has also demonstrated anti-inflammatory effects in preclinical studies.
has anti-inflammatory and antibacterial properties and may help improve focus and concentration.
has anti-inflammatory properties and may help reduce pain and muscle tension.
has anti-inflammatory properties and may help improve mood and reduce stress.
It’s important to note that the effects of terpenes may vary depending on the individual and their specific condition.
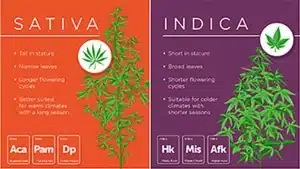
While there is no cure for IBD, medical marijuana can help alleviate some of the symptoms associated with the condition. Here are some strains that may be beneficial:
nice cerebral high helps in the proper management of symptoms related to stress and anxiety. Some patients report relief from chronic pain as well. It’s also recommended for pain management and it has been widely used for treating muscle spasms. In addition, it provides relief from physical pain and calms the mind, making it much easier for patients to manage pain.
You should remember that finding the right strain for IBD is a highly individualized process, and the optimal strain may vary depending on personal preferences and symptom profiles.
There are several online tools and resources available for individuals with Inflammatory Bowel Disease (IBD) to manage their condition and get information. Here are some of the best online tools for IBD:

Overall, these online tools provide valuable information, resources, and support for individuals with essential tremor and their caregivers, and can help them better manage their condition.
Inflammatory Bowel Disease is a complex condition that affects millions of people worldwide. The unpredictable nature of IBD like uncontrollable flare-ups and diarrhea can leave someone with IVD feeling debilitated and can affect everyday activities. However, there are various treatment options available to help manage the symptoms and improve quality of life.
Medical marijuana is one of the alternative treatments that have shown promise in alleviating symptoms such as pain, inflammation, and nausea associated with Inflammatory Bowel Disease. With its various strains and terpenes, medical marijuana can be tailored to the individual needs of patients, making it a promising option for those looking to manage their condition. If you are interested in exploring medical marijuana as a treatment option for Inflammatory Bowel Disease, book an appointment with MMJ Health, a trusted medical marijuana doctor in Florida with 9 locations.
In conclusion, if you or a loved one are seeking relief from the challenges of Inflammatory Bowel Disease (IBD), MMJ Health is here to help. With our 9 convenient locations in Florida, we are committed to providing compassionate and comprehensive care for individuals with IBD. Our friendly and knowledgeable staff, along with our team of esteemed doctors specializing in medical marijuana, are dedicated to finding personalized solutions to help manage your symptoms and improve your quality of life. Don’t let IBD hold you back any longer – take the first step towards a better tomorrow by booking an appointment with MMJ Health today. Together, we can navigate your journey towards wellness and relief.
Living with Inflammatory Bowel Disease (IBD) presents numerous challenges for individuals who are affected by this chronic condition. One of the most significant struggles faced by those with IBD is the unpredictability of the disease. Fluctuating symptoms, including abdominal pain, diarrhea, fatigue, and weight loss, can disrupt daily routines, impact work or school commitments, and strain personal relationships. The unpredictability of flare-ups and the need to constantly manage symptoms can lead to feelings of anxiety, frustration, and a sense of loss of control over one’s own body. Furthermore, the chronic nature of IBD requires long-term management, which may involve medications, dietary modifications, and regular medical appointments. Coping with these physical, emotional, and lifestyle challenges can be overwhelming, making it crucial for individuals with IBD to receive comprehensive support and guidance from healthcare professionals, as well as seek understanding and compassion from their loved ones and support networks. By addressing these struggles head-on and implementing effective strategies for symptom management, individuals with IBD can strive to regain control over their lives and find a sense of empowerment in their journey towards better health.